-
Same Day Reporting Available
-
Bulk Billing Available

1. Precise Radiology, Carnegie, Victoria, Australia
2. Western Health Medical Imaging Department, Footscray, Victoria, Australia
Ming Tan, Western Health Medical Imaging Department, Footscray, Victoria, Australia; Precise Radiology, Carnegie, Victoria, Australia.
Traumatic dislocation of the peroneal tendons is a rare injury which has been reported to occur most commonly during snow skiing or mountain climbing.1 It is a result of violent passive dorsiflexion or inversion stress, causing damage to the superior peroneal retinaculum.2 This article presents a rare clinical case of traumatic peroneal tendon dislocation resulting from a sporting injury. The anatomy, pathophysiology, ultrasound imaging technique, ultrasound appearance, grading and treatment of dislocation of the peroneal tendons are described.
The peroneus longus muscle originates in the articular capsule of the tibiofibular joint and the proximal part of the fibula. The peroneus brevis muscle originates from the distal two-thirds of the fibula and intermuscular septum, becoming tendinous 2 cm to 3 cm proximal to the tip of the fibula. At the level of the lateral malleolus, both tendons run in a common retrofibular groove, which is a fibrocartilaginous cushion. Distal to this groove, both peroneal tendons run distally and are covered by the superior peroneal retinaculum, which holds the tendons in place to reduce tendon excursions and prevent the tendons from dislocation.3 Distal to this, the inferior peroneal retinaculum covers the tendons at the lateral calcaneus. The tendon of the peroneus longus inserts at the base of the first metatarsal bone and the medial cuneiform, and the peroneus brevis inserts at the base of the fifth metatarsal bone. Together these muscles pronate the foot and support plantarflexion.4 As shown in Figure 1 the superior and inferior peroneal retinaculum cover the peroneal tendons at the level of lateral malleolus and lateral calcaneus (Videos 1 and 2).
Traumatic dislocation of peroneal tendons is a direct result of rupture to the superior peroneal retinaculum. It occurs when an acute contraction of the peroneal muscles occurs with an inverted supinated position of the foot. Mountain or rock climbers often use the big toe to keep a stand on a small rock, while the full body weight is applied to the big toe and the peroneal muscles contract to a maximum to keep a stand on a small hold. In this position the tendons are under a strong tension. If a rupture of the superior peroneal retinaculum occurs the tendons are dislocated out of the small retromalleolar groove around the tip of the lateral malleolus.5
A high frequency linear probe was used for the examination of the ankle. Ankle ligaments were examined to check for potential tear or sprain. As during inversion injuries, there is a high possibility of ankle ligaments injury, commonly involvement anterior inferior tibiofibular ligament and anterior talofibular ligament, calcaneofibular ligament.6
Then the peroneal tendons were examined for any signs of tendinitis or tendon tear with the ankle in the neutral position.
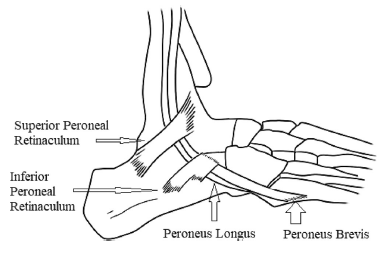
FIGURE 1 Anatomy of peroneal tendons.
Peroneal longus (PL) and peroneal brevis (PB) tendons were identified by tracing from the distal insertions of the tendons to the musculotendinous junctions. Full assessments of the tendons were performed with the main focus being over the lateral malleolar region.
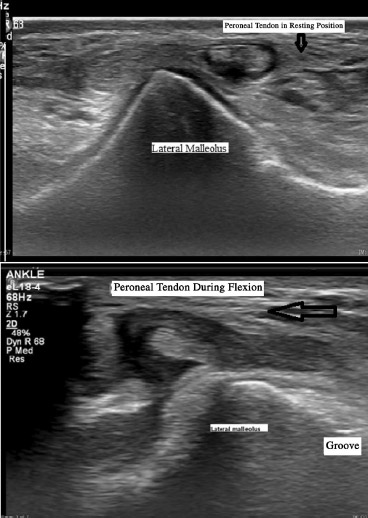
FIGURE 2 Compare the normal position of peroneal tendon and the position of dislocated peroneal tendon.
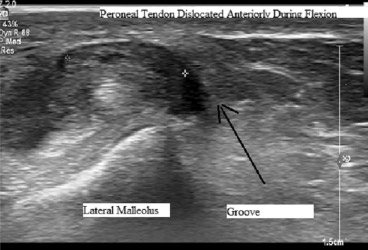
FIGURE 3 Transverse position of dislocated peroneal tendon during flexion proximal.
In additional to B-mode imaging colour Doppler can demonstrate increased vascularity changes within the tendon sheath and tendon, which helps determine the degree of activity of local inflammation of the peroneal tendons.7
To further evaluate the peroneal tendon dislocation, dynamic imaging was performed. The ultrasound probe was positioned in the axial plane of the tendons at the level of the fibular groove, followed by active manoeuvres of the ankle from the neutral position to maximum dorsiflexion position. Both peroneal tendons dislocated anteriorly over the lateral malleolus during the dynamic scan.8
Figure 2 ccompares the normal position of the peroneal tendons when ankle in neutral position to dislocated peroneal tendons during flexion.
Figures 3–7 were taken in succession from superior to inferior at the transverse plane of the peroneal tendons, at the level of lateral malleolus. As shown, the peroneus tendons were dislocated out of the retrofibular groove anteriorly to the lateral malleolus during ankle flexion
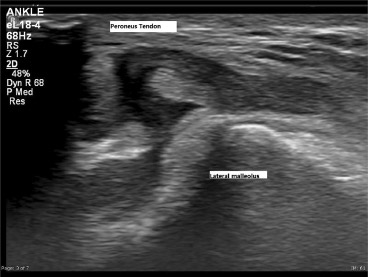
FIGURE 4 Transverse position of dislocated peroneal tendon during flexion prox/mid.
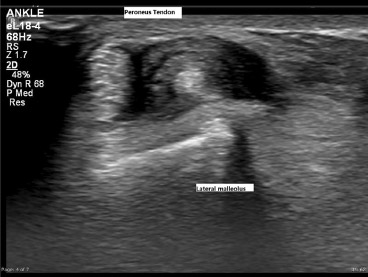
FIGURE 5 Transverse position of dislocated peroneal tendon during flexion mid
Peroneal tendon dislocation can be either acute or chronic with most acute cases being the result of athletic injuries.8 Patients often report hearing a snapping or popping sound at the time of injury
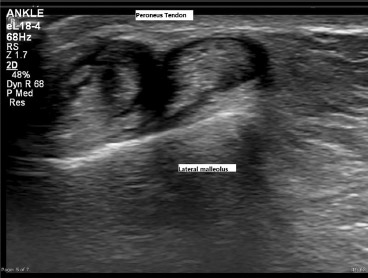
FIGURE 6 Transverse position of dislocated peroneal tendon during flexion mid/dist
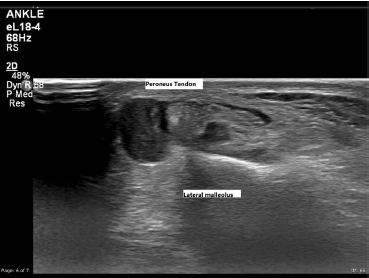
FIGURE 7 Transverse position of dislocated peroneal tendon during flexion distal
with diffuse lateral swelling and ecchymosis. These symptoms can be misdiagnosed as an inversion ankle sprain clinically, resulting in delay of treatment. Clinical correlation with the mechanical of the injury and clinical symptoms including popping or sensation of posterior lateral ankle are vital for the diagnosis1.9 Patients with peroneal tendon dislocation usually experience tenderness along the posterior border of the fibula, at and above the joint line, instead of tenderness anterior to the fibula from the common lateral ankle strain involving the anterior talofibular ligament and calcaneofibular ligament.10
The commonly used classification criteria regarding peroneal tendon instability includes three grades, published by Eckert and Davies in 1976.11 The classification was expanded to a fourth grade and a modification to Grade II was made by Oden in 1987.12 The criteria and appearance for each grade are shown in Table 1 and Figure 7
Figure 8: Peroneal tendon instability grades.
Spontaneous reduction of peroneal tendon subluxation or dislocation can occur, and may only subluxate or dislocate intermittently when specific biomechanical stresses or foot movement are involved. Dynamic ultrasound allows real time imaging of the peroneal tendon in motion, which help to diagnosis intermittent dislocation of the tendon13 Transverse plane is best suited to evaluate the relation between the peroneal tendons and the lateral malleolus.7
Beside ultrasound, other imaging modalities can be used to assist the diagnosis. The ‘fleck’ sign on ankle x-ray can indicate a bony avulsion from the fibula, which may be a sign of Grade III superior peroneal retinaculum injury.4 Magnetic resonance imaging (MRI) can be used to detect and grade any superior peroneal retinacular injuries. In addition, MRI can provide important information for presurgical planning, including common concomitant soft-tissue and osseous abnormalities of the lateral collateral ligaments, peroneal tendons, and fibular groove.14
Peroneal tendons subluxation or dislocation is relatively rare, which can be misdiagnosed as simple lateral ankle sprains.15 In order to help to improve diagnosis, a clear clinical history of the mechanic of the injury is important. The physic examination can also be used to differentiate between peroneal tendon dislocation and ankle sprain. For patients with peroneal tendon dislocation will demonstrate more posterior tenderness and fewer symptoms anteriorly, particularly over ATFL region. The anterior drawer test is negative and discomfort or apprehension is maximised by resisted eversion of the foot, which mimics the proposed mechanism of injury.16
| Grade I | Superior peroneal retinaculum is stripped from the lateral malleolus with the peroneal tendons dislocated into the space between the eriosteum and fibula. |
| Grade II | The fibrocartilaginous ridge is avulsed from the superior peroneal retinaculum, and the peroneal tendons are dislocated between the fibrocartilaginous ridge and the fibula. |
| Grade III | A bony avulsion from the fibula with superior peroneal retinaculum injury. The peroneal tendons are dislocated between the fragment and the fibula |
| Grade IV | The superficial peroneal retinaculum is torn from its posterior calcaneal attachment and deep investing fascia of the Achilles tendon. The peroneal tendons are dislocated superficially to the superficial peroneal retinaculum. |
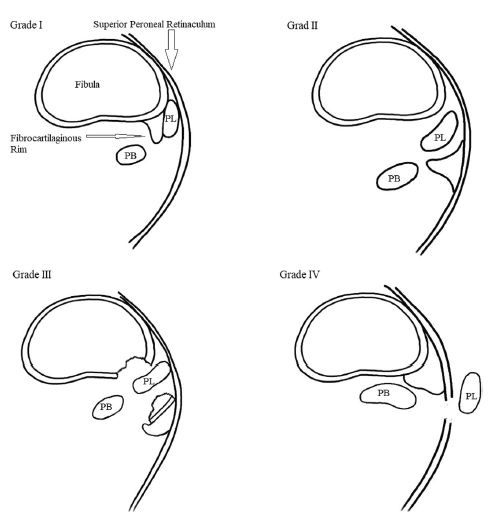
FIGURE 8 Four grades of peroneal tendon dislocation.
Conservative treatment of acute peroneal tendon dislocation includes cast immobilisation, reducing tension on the tendons by heel lifting, taping of the ankle, rehabilitation, and orthotics.9 However conservative treatment tends to have a low success rate and can cause chronic instability of the ankle joint. Surgical procedures of various techniques to reconstruct the superior peroneal retinaculum have resulted in excellent recovery rates and faster return to professional sport.17
In this case the patient had been placed in a cast for 6 weeks, followed by physiotherapy after removing the cast. Full recovery was achieved
Traumatic dislocation of the peroneal tendons is a rare injury that results from the rupture of the superior peroneal retinaculum. It can occur during sporting activities such as rock climbing when there is a high force impact onto the superior peroneal retinaculum resulting in rupture of the superior peroneal retinaculum or avulsion of the fibrocartilaginous ridge. Dynamic ultrasound is an effective and cost-efficient tool for diagnosing peroneal tendon dislocation, which can help the clinician to provide correct management and treatment to the patient in a timely manner.
The author would like confirm upon submission that informed consent to publish has been obtained from the patient who are involved in this case study and thanks for the patient’s support of the writing and publishing of this case study. The author would like to express his special thanks and acknowledge the help and contribution of: Mr Adam Steward, Radiography Tutor of Western Health Medical Imaging Department for the internal reviews of the article. Mr Jason Heidrich Chief Radiographer of Western Health Medical Imaging Department Footscray Hospital, for approval and support of the article. Ms Sandra McConville, Clerical Supervisor of Western Health Medical Imaging Department, for help obtain the written consent. Miss Yongying Han, author’s wife, for the illustrate drawing of the anatomy of the peroneal tendon and peroneal retinaculum; and the classification grades of peroneal tendon instability.
The article is funded by Author.
The authors declare that they have no conflicting interests..
Ming Tan https://orcid.org/0000-0002-3897-2150
Additional supporting information can be found online in the Supporting Information section at the end of this article
How to cite this article: Tan M. Traumatic dislocation of the peroneal tendons. Sonography. 2024. https://doi.org/10.1002/sono.12400