-
Same Day Reporting Available
-
Bulk Billing Available

Medical Imaging Department, Western Health, Footscray, Victoria, Australia
Ming Tan, Medical Imaging Department, Western Health, Melbourne, VIC, Australia.
Common peroneal nerve (CPN) neuropathy resulting in foot drop is a relatively uncommon complication of patients who are positioned in the lithotomy position during surgery, and the most common cause of spontaneous painless foot drop.1 Although diagnosis is often based on the clinical findings, ultrasound can be used as an efficient and effective imaging tool to identify the cause of CPN neuropathy and other peripheral nerve disorders. In this article, two ultrasound cases of patients with post operation foot drop as a result of CPN neuropathy are presented. The anatomy, ultrasound imaging technique, ultrasound appearance of CPN neuropathy; and potential causes of CPN are described.
The CPN, also known as the common fibular nerve, is the lateral division of the sciatic nerve (Figure 1). The sciatic nerve bifurcates into the tibial and peroneal nerves proximal to the popliteal fossa.2 The CPN courses from the posterolateral side of the knee around the biceps femoris tendon and the fibular head to enter the lateral compartment of the leg.3 Just inferior and lateral to the fibular head, it divides into three nerves at the fibular neck region including the superficial peroneal nerve, the deep peroneal nerve and a small recurrent articular branch.4
Ultrasound examination of the CPN involves the use of a high frequency linear transducer. The patient is placed in the prone position. The scan is started at the posterior distal thigh, to identify the sciatic nerve which is then traced inferiorly to its bifurcation. The CPN is the more lateral and smaller branch of the sciatic nerve. The entire length of the CPN is traced to its distal trifurcation at the level of the fibular neck. Colour Doppler can be used to help differentiate nerves from vessels.
The normal CPN has a ‘honeycomb-like’ appearance in transverse section and a ‘bundle of straws appearance in longitudinal section, which has hypoechoic areas separated by hyperechoic septation. The hypoechoic areas represent nerve fascicles, while the echogenic septation represent interfascicular perineurium, as shown in Figure 2.5–7
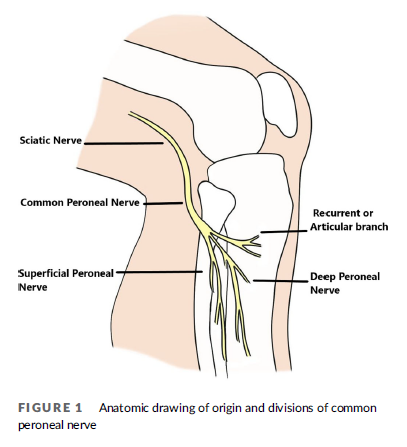
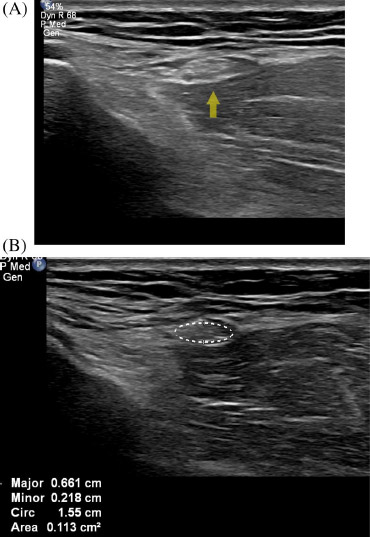
FIGURE 2 (A) Normal right common peroneal nerve at the level of the neck of the fibula. Arrow denotes nerve. (B) Normal right common peroneal nerve in cross-section (denoted by ellipse tracing)
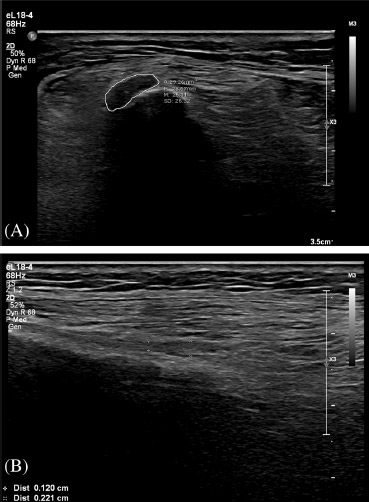
FIGURE 3 Images from a 61-year-old female patient with left foot drop (Case 1). (A) Shows a focally thickened and hypoechoic left CPN at the fibular neck (ellipse tracing). (B) Longitudinal image of common peroneal nerve at the fibular neck demonstrating focal distal thickening
Neuropathy of the CPN can result in foot drop, weakness of other muscles group controlled by the CPN including the extensors of the toes and peroneus muscles and sensory symptoms such as pain and paraesthesia.8 The CPN is responsible for innervating the anterior and lateral muscular compartments of the lower extremity, which include the tibialis anterior muscle, the extensor hallucis longus muscle, and the extensor digitorum longus muscle of the anterior compartment, and the peroneus longus muscle and the peroneus brevis muscle of the lateral compartment. The anterior compartment is responsible primarily for the dorsiflexion of the foot and the lateral compartment is responsible primarily for the eversion of the foot.4 The common site of CPN compression is at the fibula head and neck region.9
A 61-year-old female patient presented with newly developed left foot drop, reduced leg muscle power and the sensations of the left leg, at day 7 post left total hip replacement surgery.
Sonography demonstrated a focally thickened and hypoechoic CPN at fibular neck, with a cross-sectional area of 29 mm2 (Figure 3).
Subsequently, the patient reported the foot drop symptoms were resolved after 1 month at outpatient appointment
A 27-year-old male patient presented with newly developed left foot drop post open reduction internal fixation surgery of a left proximal tibial fracture. On ultrasound examination, a focal thickening of the CPN at the level of the fibular head was demonstrated. The extensor hallucis longus and extensor digitorum longus tendons appeared intact.
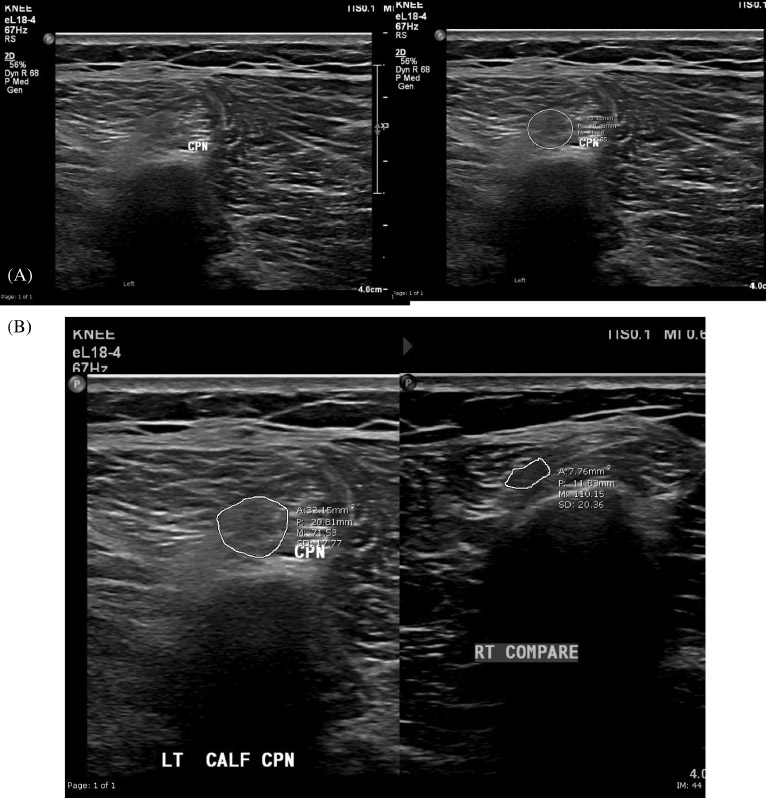
FIGURE 4 Images from a 27-year-old male patient with left foot drop. Sonography demonstrated a focally thickened and hypoechoic CPN at fibular neck, with a cross-sectional area of 33 mm2 . (A) Focally thickened and hypoechoic left common peroneal nerve in cross-section (ellipse tracing). (B) Comparative image of the normal right CPN in cross-section
Sonography demonstrated a focally thickened, oedematous and hypoechoic CPN with a cross-sectional area of 33mm2 (Figure 4).
On follow-up of the orthopaedic clinic review, the patient still presented with minor neurological symptoms of the foot, and the patient was referred for ongoing physiotherapy treatment.
In both of these cases, the nerve lost the normal honeycomb-like appearance on ultrasound and became uniformly hypoechoic, which is due to loss of the normal fascicles and damage to the epineurium.10 No colour flow was seen on Doppler ultrasound
The ultrasound images had demonstrated focal thickening of the CPN at the fibular neck with increased cross-sectional areas (Case 1 Figure 3A, 29 mm2 and Case 2 Figure 4A, 33 mm2 ), compared to the normal CPN (Figure 2A). Multiple studies illustrate that upper limit cut-offs values for CPN cross section area ranges from 11.7 to 26.2 mm211–13 and can be used to differentiate normal CPN from neuropathy of CPN. A cut cuff value of 11.7 mm2 has shown a high sensitivity of 85.0% and high specificity of 90.0% from the most recent research.11 Using these criteria, the CPNs described in these two cases are not of normal size
In addition to ultrasound, electrodiagnostic testing, which includes nerve conduction studies (NCS) and needle electromyography (EMG) can be performed to confirm the location of neuropathy.14
Both cases developed CPN neuropathy after orthopaedic surgery. The aetiology of this type of postoperative neuropathy is multifactorial, although most cases are thought to be attributed to patient positioning, compression, or stretching of nerves and inadequate protection of susceptible sites.15 Prolonged compression during orthopaedic, gynaecologic and abdominal surgeries with operative positioning of lateral hip and leg rotation with knee flexion or the lithotomy position can result in peroneal nerve injury. In addition to that, patients who require prolonged bed rest after surgery may also be at risk for peroneal neuropathy.16 Several risk factors have been implicated in lithotomy position-related CPN neuropathy during operation. When the CPN exits the popliteal fossa, the common peroneal nerve crosses the lateral head of gastrocnemius and popliteus and wraps around the fibula neck in order to enter the lateral compartment of the leg.17 Around this area, the CPN is exposed over a bony prominence covered superficially only by subcutaneous fat and skin for a length of 4 cm. The CPN also has limited longitudinal mobility where the nerve is in a relatively fixed position from its origin at the sciatic nerve to the trifurcation at the level of the fibular neck. All these factors together make the CPN susceptible to external compression or other injury over this region.9,18,19
To help to reduce the incidence of neuropathy of the CPN, for operations with patients in the lithotomy position, or other positions that involve fixation of the leg, the fixing duration should be reduced in order to prevent postoperative neurologic complications.20 Studies illustrate that the risk of motor neuropathy is increased by 100 times as the external fixation time increases by 1 h.18,21
The symptoms of the patient in case 1 resolved after 1 month. For case 2 the patient’s symptoms had nearly resolved after been treated with physiotherapy for 4 months. Studies have demonstrated that there are high rates of spontaneous recovery of CPN palsy with conservative management in cases where the causative mechanism was compression.9
Many patients will experience spontaneous recovery early in the course, and hence observation and symptomatic treatment is the first line of management. For those patients who do not spontaneously improve, surgical decompression is a safe and effective treatment option.4,22
Post-operative neuropathy of CPN resulting in foot drop is a rare surgical complication. It is commonly caused by prolonged compression of the CPN at the region of neck of fibular from the fixed position. Ultrasound can effectively assess CPN neuropathy in patients with foot drop. Although CPN neuropathy will recover spontaneously in most patients, surgical decompression should be considered for patients with persistent neuropathy.
The author would like confirm upon submission that informed consent to publish has been obtained from the patients who are involved in this case study and thanks for the patients’ support of the writing and publishing of this case study. The Author would like to express his special thanks and acknowledge the help and contribution of: Mr Adam Steward, Radiography Tutor of Western Health Medical Imaging Department and Ms Renee Mineo, General Radiography Supervisor of Western Health Medical Imaging Department, for the internal reviews of the article. Ms Nicole McDonald, Chief Sonographer of Western Health Medical Imaging Department and Mr Jason Heidrich Chief Radiographer of Western Health Medical Imaging Department Footscray Hospital, for approval and support of the article. Ms Sandra McConville, Clerical Supervisor of Western Health Medical Imaging Department, for help obtain the written consent. Miss Yongying Han, author’s fiancée, for the illustrate drawing of the anatomy of the common peroneal nerve.
The article is founded by Western Health Medical Imaging Department, Victoria
The authors declare that they have no conflicting interests.
Recorded informal consents were obtained from the patients, for the purpose of publication of this case report and any accompanying images.
Ming Tan https://orcid.org/0000-0002-3897-2150
How to cite this article: Tan M. Post operation neuropathy of common peroneal nerve resulting in foot drop. Sonography. https://doi.org/10.1002/sono.12359